Pressure-Volume Loops (PV Loops) are a very useful tool during
hypothetical analysis of a
chamber of the heart. This refers to
any chamber of the heart (RA, RV, LA, or LV). This will be a picture-heavy post, but let's get a better understand of just what the PV Loops is designed to tell us!
Let's just start with a quick look at what a
PV Loop looks like:
There it is in its glory, Not much to look at, eh? Don't worry! With the use of my laptop, let's get a few things labelled so that the
PV Loop is a lot less
mystery and a lot more
awesomely useful.
Let's start with the axes:
Just for clarity, the
x-axis depicts
volume, while the
y-axis depicts
pressure.
This
line shown in the
PV Loop is a depiction of
contractility. Shortly, you will get a chance to see how a
change in
contractility (via that line)
alters the shape of the
PV Loop.
The
width of the
PV Loop corresponds to
stroke volume. Just like
contractility, you will shortly see how easily the
stroke volume can be
altered by the shape of the
PV Loop.
Now, for big concepts: A
PV Loop depicts the events of a
single, hypothetical heartbeat. What is also true is that the
PV Loop is not a '
snapshot' of the heart. To read the
PV Loop, you must
travel along the
PV Loop. Does that make sense? What I mean is, you pick a point to start (let's say the
Upper Left corner, and then
follow the loop's
line. Something that is true is that
throughout that
heartbeat, the
pressure is
always changing. As you
follow the
line of the
PV Loop, you
never just stay at the same
value along the y-axis (the axis that depicts
pressure). You may
return or have
similar pressure value
eventually, but you are just
stuck at one particular value of
pressure. How does this apply to the x-axis (the axis that depicts
volume)? Excellent! There are
two points in time in which the
volume in the heart is
unchanging (depicted by the two
vertical lines, one on the
left and another on the
right of the
PV Loop). There are
two points in time (within the
heart) that the
volume is
unchanging, one (the
left) value is
isovolumetric relaxation and the other (the
right value) is
isovolumetric contraction. We will come back to both, shortly.
Here are some of the
major events within the
left ventricle. Remember, that the
PV Loop can depict activity in
any of the
four chambers of the
heart. In our example, we are talking
specifically about the
PV Loop in the
Left Ventricle. Let's start in the
Upper Left corner of the loop. At this moment, I have denoted that the
aortic valve closes. The
aortic valve is the
valve that exists in the
aorta, and can
allow or
prevent communication between the
LV and the
body. As a
result of the
aortic valve closing, the chamber exists in a state in which
no valves are open. I will follow with a labelled picture, but the
left vertical line of the
PV Loop depicts, then, a time of
isovolumetric relaxation. Picking apart the word,
isovolumetric relaxation refers to a period of
relaxation in the
heart in which there is
no change of volume occurring (a
result of the fact that
no heart valves are
open).
At the
Bottom Left corner of the
PV Loop, the
mitral valve opens. Remember, the
mitral valve is the valves that separates the
left atrium from the
left ventricle. What do you suppose happens when the
mitral valve opens and allows communication between the
LA and the
LV? Of course! When the
mitral valve opens blood is allowed into the
left ventricle and
diastolic filling of the
chamber begins! Great job!
At the
Bottom Right corner of the
PV Loop, the
mitral valve closes. Here we are again, with
none of the
heart valves that communicate with the
LV being
open. Again,
no change in
volume occurs, making this
isovolumetric. This time, however, rather than
relaxation occurring,
contraction is occurring. What's the
difference, or what makes one
relaxation and the other
contraction? I'm glad you asked! So, let's start with
isovolumetric contraction (the
right vertical line). What has occurred in the heart (due to
diastolic filling)? It's filled with blood! Something we have
yet to discuss is that there is
electrical activity going on within the heart (preparing the
heart to
contract for a
heartbeat). So, as the
cardiac myocytes begin to
contract (or,
shrink in size), that
pressure, combined with the
pressure created by the
stretching of
cardiac myocytes due to being filled with blood,
continually increases. In contrast,
isovolumetric relaxation (the
left vertical line) is occurring
after contraction (or
ejection of blood from the heart) has occurred. As you can imagine, that is a huge
relief or a
relaxing event for the heart. It's allowed to
return to its
normal, original size. I will be providing a labelled diagram of this in just a sec, but I think the next paragraph will help here.
Finally, at the
Upper Right corner of the
PV Loop, the
aortic valve opens. Now, what happens in the heart? Right! When the
aortic valve opens (alongside that
contraction of the
left ventricle) blood is
ejected from the
heart to the
aorta (to be carried to the
body). Starting the
Bottom Right corner and ending with the
Upper Left corner, we have described
contraction (or the period of
systole in the heart).
Now, for some labelled diagrams:
And, to just be even more helpful (I know my artwork is
terrible), here's a
professional depiction of the
PV Loop, with all of the bits and pieces labelled (I just wanted to go slow, initially). If you are confused (as I feel that I may not have done as well as I could have, please leave a comment):
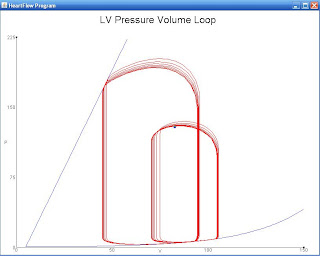
So, know, let's look at how
fairly isolated changes in
preload, afterload and
contractility can affect the
appearance of the
PV Loop.
Here's a
fairly isolated change in
Preload:
What
changes do you see between the
normal loop (more to the
left) and the loop with increased
preload (more to the
right)?
Did you see any of these changes? As noted, an
increase in
preload is going to result in an
increase in
stroke volume! But, we already knew this, and we certainly didn't need a
PV Loop to explain the relationship. If
preload were to increase, the amount of
blood that fills the
left ventricle during
diastole is going to increase (
see the notation of the end volume in appropriate colors). As a result, when that
blood is
ejected from the heart,
more blood will be ejected (or a
higher stroke volume will be ejected). What are some things that might
increase preload? Well,
fluid retention or
fluid administration is an easy way to
increase preload in the body. A
decrease in
preload (not depicted) might result from
blood loss or even the use of
diuretics (Lasix).
How about this
fairly isolated change in
afterload? What changes do you see in this
PV Loop?
Did you see these changes:
So, what do we see with this
fairly isolated increase in
afterload. Again,
stroke volume is affected. However, this time
stroke volume has
decreased in response to the
increased afterload. But, then again, we already knew that too! If
afterload were to increase, the
force that the
left ventricle would have to overcome to
eject blood would also
increase. Because of this, the
LV is going to have to do
more work in order to
compensate for this increase in
resistance. Note, again, the changes along the axis. On the
y-axis, one can see that the
initial SV results in smaller amount of
pressure being exerted, when compared to the
second PV-Loop. Certainly, that
increased pressure reflects that increased
resistance or
load that must be
overcome for blood ejection. What might cause an
increase in
afterload? Well, if we had taken this
PV Loop measurement
right as or
fairly soon after the
aorta had
stenosed (or
collapsed), we might see an
increased afterload like this.
And our final loop, a change in
contraction (thus far we've had
no change in contraction):
Wow! There are some drastic changes in the loop with this change in contractility. What things do you see?
Some
notes on the
effects the
change in contractility have had on this loop. First, the
slope of the
contractility line has
decreased. The decrease in
slope corresponds to a
decreased contractility. Look at the
stroke volumes. In the
initial heart
PV Loop, the
SV is
much greater than the
stroke volume created by the
second PV Loop.
So, what might cause changes in
contraction (such as these)? Well, let's say on the
initial loop (the one to the
left), it was taken while I was
running from a
monster (high
contraction going on). The second loop (or the loop to the
right) might have been taken
after I had been given a
sedative by a doctor, following my
intense run in with a
monster. Here, the
sedative has decreased
contraction in my heart.
There you have it! That was a
whole lot about the
PV Loop. If you are interested in a
great simulator for the
study of the heart, here is a
FANTASTIC website:
http://ccnmtl.columbia.edu/projects/heart/sim.html. Here you will find the method that allowed me to make this post.
The
PV Loop, once you understand and get past the
WOW factor (and by WOW, I mean, "WOW, what is this
mumbo jumbo??"), can be quite helpful in making diagnoses. Something that I have yet to note (or I should say
stress) is that the
PV Loop makes
no consideration for an
increase in
wall thickness. It couldn't, right? The
PV Loop is a measurement of
only one heartbeat. As we have seen,
wall thickness is something that
changes over a
long period of time. Also in need of note, while I
proposed to you some '
isolated' changes in some of the values, this really is
not going to happen in the heart. Why? Well, that's because the heart has those
Top 3 Priorities, and it is
always changing things (
all things) to
ensure that those priorities
are met.
Cheers (and believe me when I say, this will definitely need a reread once I have slept some)!
** Reread and improved at 5:00 PM the next day **